In the late 1980s I read about the progress being made with insulin pumps. They had become smaller in part due to learning from the US space program. The Diabetes Treatment Center of Atlanta was progressive and an excellent resource for insulin pumps. I researched the handful of available pumps and asked my endocrinologist at the time, Paul Davidson, the pumps I should evaluate. He said that he recommended and worked with only one provider, Minimed. (Hmm … that raised my eyebrows, but I followed his lead.)
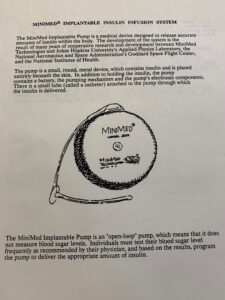
But within MiniMed there were two options – an external pump and an implantable one. What, an implantable pump? It was the size of a hockey puck … he asked if I was interested. Here’s the front page of the info packet I was provided:
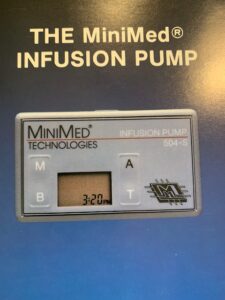
When I asked how the pump would be refilled with insulin, Dr. Davidson said it was injected periodically with a long syringe through my stomach. Say that again? I don’t think so! That was a deal breaker for me and my answer was to go with the external Medtronic pump, the 504S.
The 504S was about the size of a 1980s pager. To get started, I spent two days at West Paces Ferry hospital in order to determine my basal profile. Pat Richardson was a Certified Diabetes Educator and was terrific in many ways. On top of her great bedside manner, she was knowledgeable and a great teacher of how to use the pump.
As for the 504S, it had benefits and drawbacks.
On the plus side, the basal profile provided really good results at night while sleeping. I could go to bed with a blood sugar of 100 and wake up very close to that same number. Those results were far better than the inconsistent results from NPH insulin.
The drawbacks for me were many:
- The pump was not waterproof and had to be put into a sealed watertight pouch when close to water. Wearing the pump when swimming or during other water wasn’t feasible.
- Unlike later models, the infusion set didn’t have a disconnect port. Therefore, my day started with putting the insulin pump in a waterproof pouch and wrapping the infusion set tubing around my neck so I could shower.
- The infusion set was inserted with a long steel needle. It usually hurt going in, remained there for 2-3 days and was covered with medical dressing called Tagaderm. Many times it was sensitive to touch. I remember walking through the busy Atlanta airport protecting my infusion sight for fear of being bumped. On another occasion, I went snow skiing and rolled down a slope after falling. I was surprised that my infusion sight had stayed in.
- Socially, I was conscious about being ‘connected’ to the pump. I wasn’t prepared to explain it when playing sports, dating, and the questions at work.
- I experienced consistent hypoglycemic episodes during afternoons. Finally, Dr. Davidson recommended that I change my afternoon and early evening basal rate to 0.
For these reasons I chose to go off the pump in 1990 after about a year. The pump went back in the box and stayed there until my nephew used it as a substitute for his co-pay on a pump fifteen years later.
I made the decision that was right for me at the time. The concerns I had with the pump (inconvenience and psychosocial) went away as I put it back in the packing case. And I continued to live life with multiple daily injections (Regular and NPH insulins), albeit with more nocturnal blood glucose roller coaster rides.
————————-
Flash forward 16 years to 2006. After going on the first generation Dexcom CGM, I noticed my glucose levels rising 3-4 hours after injecting Humalog for meals. So, I approached my endocrinologist about going back on the pump. A decade and a half later, a lot had changed:
- I was married
- I was a father
- My career had taken off and I had key responsibilities – and stress – in business.
- Humalog replaced Regular insulin. Humalog acted quicker and had a shorter active insulin duration.
- Infusion sets had a disconnect port and were much less intrusive when showering, swimming and during intimacy.
- I found a confidence and voice for diabetes, becoming active with the Kansas City JDRF chapter and talking with others whose lives were affected by type 1.
After spending a week or so getting the bolus and basal profiles right, I was back on the pump. Have been even since. While my A1Cs didn’t improve, the quality of my life did:
- I slept better.
- My lows were fewer … and more predictable.
- Exercising became more enjoyable as I discovered that it was best with little active insulin. I could reduce the amount of basal insulin before and during exercise.
- I had more consistent blood sugars … improving my moods and relationships at work, home and with friends.
So there you have it. Two different attempts at pumping with different results. I don’t think there is a ‘right’ answer as to pump or do multiple daily injections. I did what I thought was right for me each time.
I am grateful for the inventors of the miniaturized insulin pumps of the 1980s. They customized insulin infusion in a wearable solution that improved the quality of life for people with type 1 diabetes. I am equally appreciative of the innovation from the pump companies that came in the second wave of competitive pumps. The innovation and competition from Animas, Deltec, Medtronic, Omnipod, Roche and Tandem brought new features (e.g. bolus wizard calculations, extended boluses), data (active insulin, daily averages, uploads) and styles (attached, no infusion sets, touch screens) that expanded choices for people living with diabetes. In addition to the features and choices these pumps provide, I must add that some of today’s pumps have what I consider a ‘cool factor’ that I never thought I’d see in a medical device. We’ve come a long way baby!